A pilonidal sinus is tucked away in the body’s most unspoken area and is rarely brought up at dinner parties or in casual conversation. However, it causes chronic discomfort, recurrent infections, and in many cases, excruciating pain for thousands of people every year. The condition may seem insignificant at first, but it has a significant impact on day-to-day living. Thankfully, medical advancements in recent years have changed the way this issue is handled by providing a minimally invasive and remarkably effective surgical option that is revolutionizing the treatment of patients all over the world.
Surgeons can now clean the infected sinus without making large incisions or staying in the hospital for a long time thanks to high-definition endoscopes and improved techniques. These developments provide a very effective substitute for open surgeries. Most of the time, patients are given spinal or local anesthesia, have the procedure done in less than an hour, and go home that same day. Thanks to precision tools and enhanced aftercare protocols, wounds that previously required weeks of care and follow-ups can now heal in as little as two to four weeks.
Pilonidal Sinus Surgery – Key Details
| Category | Information |
|---|---|
| Procedure Name | Pilonidal Sinus Excision or Endoscopic Cleaning |
| Method | Endoscopic sinus removal + hair extraction + heat or glue sealing |
| Anesthesia Type | Local or spinal (outpatient) |
| Recovery Duration | Typically 2–4 weeks (may vary based on individual healing) |
| Restrictions After Surgery | No heavy lifting, biking, or swimming for 6–8 weeks |
| At-Risk Population | Primarily young men, those with sedentary jobs or dense body hair |
| Complication Risk | Exceptionally low with modern minimally invasive methods |
| Preventive Practices | Hygiene, regular hair removal, avoiding prolonged sitting |
| Trusted Resource | NHS Guide to Pilonidal Sinus Treatment |
| Celebrity Mention | While not publicized, athletes and actors reportedly undergo similar procedures for fast recovery |
Hair, Stress, and a Secret Issue: Determining the Cause
Pilonidal sinus disease is an odd example of a medical condition that appears to be straightforward. This disorder causes an infection-prone tunnel in the natal cleft and is brought on by hair, friction, and extended sitting. Bacteria are introduced beneath the skin by loose or embedded hair follicles, resulting in abscesses that frequently burst, drain, or swell. Although anyone can get it, people who have thicker body hair or have desk-bound routines are more susceptible. Though strikingly similar to ingrown hairs, it is much more obstinate and may recur for years if treatment is not received.
Sedentary behavior increased among a large portion of the population during the pandemic. Sitting for extended periods of time with bad posture has become commonplace for people who work remotely. Although they are still rarely discussed, pilonidal issues became more prevalent in this setting. However, as treatments become noticeably more effective and recovery times become shorter than a long weekend vacation, that silence is now giving way to transparency.
The Procedure That Isn’t Actually a Procedure—At Least Not Like You Recall
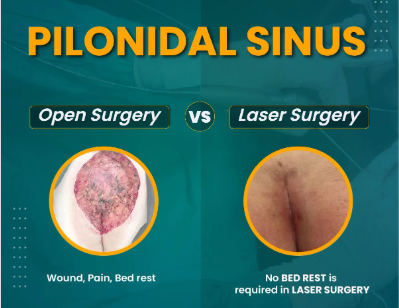
The days of frequent dressing changes, weeks off from work, and large wounds are long gone. Surgeons can now see the sinus tract with remarkable clarity, clear debris, and seal the passage with heat thanks to endoscopic techniques. Some clinics may choose to use phenol or fibrin glue instead, which provide comparable outcomes with less recovery time. In addition to being extremely effective, these new methods lessen the possibility of recurrence, which was a worry for patients in earlier decades.
Hospitals have greatly decreased complication rates by implementing this technology, which also allows patients to take charge of their own recuperation. In contrast to more invasive procedures, patients frequently return to walking in a matter of hours with little to no scarring and only mild soreness.
Actual Recuperation: How It Feels After
The procedure changed the life of 24-year-old graphic designer Hassan Ali. I dreaded sitting at my desk in the past. I would work nonstop and take 15-minute breaks. My creativity was being sapped by the pain,” he said. “It was like getting my focus—and life—back after the surgery.” His experience is remarkably similar to that of many young professionals who unknowingly increase their risk by spending a lot of time in front of their computers.
Even though the healing process is comparatively quick, attention is still needed. Patients are encouraged to eat more fiber, wear loose-fitting clothing, and maintain a clean, hair-free environment. Walking and mild exercise are advised in the beginning, but swimming, cycling, and weightlifting should be avoided for a few weeks. In order to make sure the site is healing as planned, follow-up appointments typically take place within six weeks.
A Change in Approach: The Importance of Prevention
Despite the remarkable effectiveness of surgery, prevention is still crucial, particularly for those who are genetically or occupationally predisposed. Ergonomic seating, regular hair removal, and daily natal cleft cleaning can all be beneficial. Small adjustments, such as standing desks or taking regular breaks, can also greatly lessen pressure buildup and friction for people who work from home.
Patients can embrace long-term relief and prevent repeat procedures by remaining vigilant even after a successful course of treatment. Experts stress that integrating advanced care with basic lifestyle practices yields the best results.
