For those who struggle with extreme obesity, losing weight can be likened to chasing a moving target, which is frustratingly unattainable even after a great deal of effort. Exercise regimens stall, diets change, and the health effects keep getting worse. SADI surgery has come to light as a particularly creative remedy in this environment of trial and error. With its exceptionally successful outcomes and lower risk of complications, this procedure—formally known as Single Anastomosis Duodenal Switch—is subtly but steadily revolutionizing bariatric medicine.
SADI provides a highly effective alternative for patients with a BMI of 40 or higher by combining the advantages of a sleeve gastrectomy with a simplified intestinal bypass, particularly for those who are treating type 2 diabetes, sleep apnea, or high blood pressure. SADI minimizes long-term risks while maintaining important digestive functions, in contrast to more involved surgeries. Patients are gaining control, clarity, and confidence in their future in addition to losing weight.
SADI Surgery – Key Clinical and Procedural Details
| Category | Information |
|---|---|
| Procedure Name | Single Anastomosis Duodenal Switch (SADI) |
| Target Group | Patients with class 3 obesity (BMI ≥ 40) |
| Main Technique | Combines sleeve gastrectomy with a single-loop intestinal bypass |
| Weight Loss Outcomes | Up to 80% of excess weight lost; results sustained over 5–10 years |
| Diabetes Remission | Particularly effective in reversing type 2 diabetes |
| Digestive Preservation | Pyloric valve preserved; lowers bile reflux and dumping syndrome |
| Surgical Risk Profile | Reduced leaks, hernias, and ulcers compared to other bariatric options |
| Recovery Timeframe | 2–3 weeks for most; varies by individual and follow-up care adherence |
| Insurance Landscape | Coverage expanding, though still limited across many providers |
| Verified Resource | Duke Health Bariatric Surgery |
A Fine Balance: Preservation and Restriction
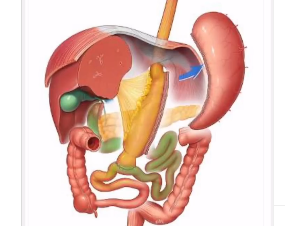
SADI’s fundamental mechanism is both transformative and accurate. To create a narrow, sleeve-shaped pouch, surgeons start by excising about 80% of the stomach. By lowering food volume capacity, this promotes early satiety. The duodenum is then redirected to a lower portion of the small intestine through a single anastomosis. This preserves the pyloric valve, a structure essential to controlling stomach emptying, while permitting partial absorption.
SADI surgery provides a very evident benefit by incorporating this valve: patients are spared the unpredictable fluctuations in blood sugar and nausea that come with dumping syndrome. Additionally, the likelihood of bile reflux, a problem that many gastric bypass patients face, is significantly decreased by this anatomical preservation. With fewer compromises, the design is noticeably better and built for sustainability and long-term comfort.
Actual Outcomes: Not Just Weight Loss
Following SADI, weight loss is remarkably consistent. Excess body weight decreased by almost 80% in clinical trials, and long-term outcomes remained consistent even ten years later. However, success isn’t defined by weight alone. SADI’s impact on related conditions is what makes it especially advantageous. Following surgery, many patients experience a reduction in blood pressure, a decrease in cholesterol, and the elimination of diabetes symptoms, turning chronic threats into conditions that can be managed or resolved.
These figures are frequently emphasized with human depth in personal narratives. The shift was “night and day,” according to 42-year-old Raleigh patient Jessica Ramirez. She struggled to climb a flight of stairs and was taking five medications before surgery. She is off insulin, hiking once a week, and pain-free at her son’s soccer matches just eight months after SADI. Despite being extremely personal, her experience is remarkably similar to hundreds of others nationwide.
Eating, Dedication, and the Path Ahead
A dedication to lifelong nutritional mindfulness is necessary for SADI. Patients must follow a structured supplement regimen because the bypassed intestine decreases absorption of certain nutrients. Usually checked by routine blood work, this includes iron, vitamin D, calcium, and B12. Even though there is less chance of malnutrition than with more drastic procedures, diligence is still crucial.
Through close collaboration with surgical teams and dietitians, patients receive customized plans that support their body’s changing needs. Like brushing your teeth or taking your morning meds, these new routines tend to become second nature over time.
Obstacles and Advancements: Access and Insurance
Insurance coverage is one of the few obstacles SADI must overcome. Even though the American Society for Metabolic and Bariatric Surgery supports the procedure, many insurance companies are still unaware of it. For example, Blue Cross and Blue Shield of North Carolina are early adopters, but in order to gain access across the country, greater recognition is required. However, coverage is anticipated to grow considerably over the next few years as results data mounts and public interest increases.
In the meantime, technical accuracy is required for the procedure itself. Only highly skilled bariatric surgeons should attempt this procedure due to the complexity of the duodenal anatomy. Thankfully, SADI has been performed for years by surgical teams at prestigious institutions like Duke and Cleveland Clinic, who have streamlined procedures and improved patient education to further lower risks.
Towards the Future: An Innovative Future
It is anticipated that SADI will continue to develop in the upcoming years. AI-driven surgical planning, real-time imaging, and robotic assistance could soon improve post-operative results and procedural accuracy. With the help of these advancements, SADI should become even safer, quicker, and more flexible for patients with different anatomy and medical histories.
Clinics are developing comprehensive programs that not only reduce weight but also maintain wellness by utilizing multidisciplinary care, combining surgical expertise with behavioral support and nutritional science. The ability of SADI to change the emphasis from scale-based victories to systemic health transformation is what gives it its holistic value.

1 Comment
Pingback: Discover Why Nail Treatments Edinburgh Are Becoming the City's New Obsession - White Nails